

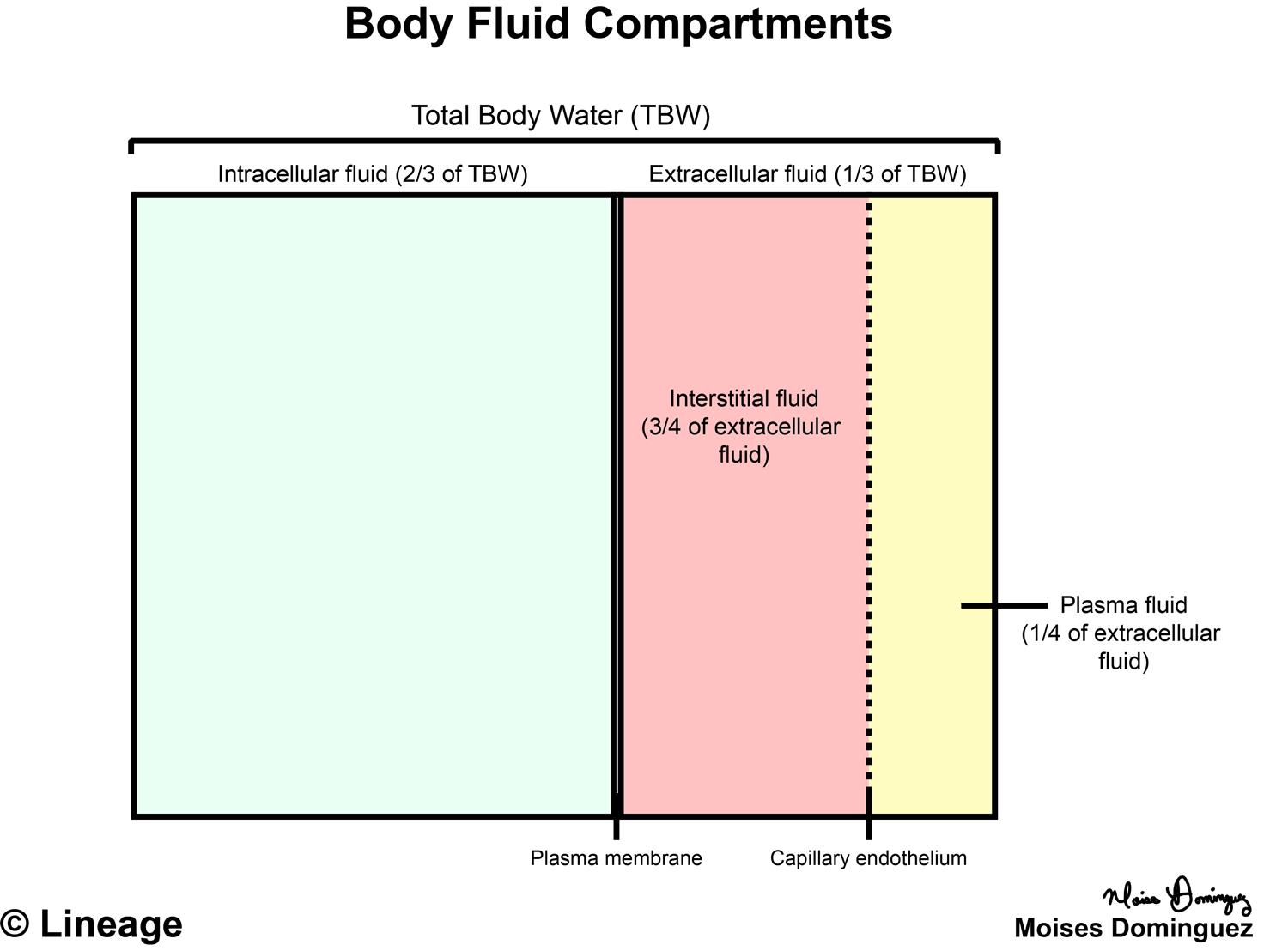
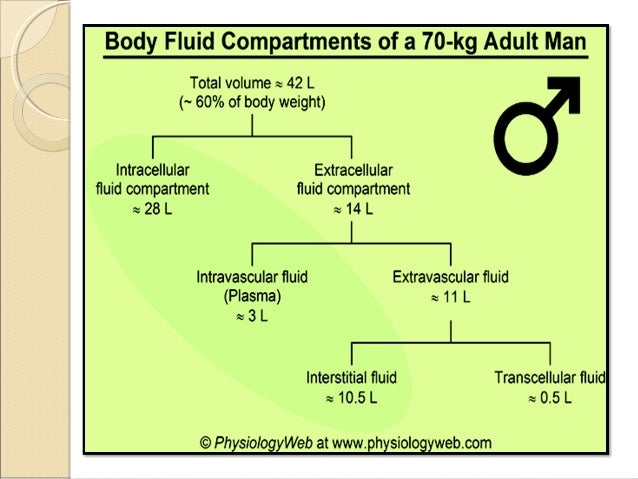
1 Osmotic pressure is the potential pressure of a solution directly related to its solute concentration. Osmotic pressure is the primary determinant of this exchange. Osmolar, hydrostatic, and oncotic pressures all regulate the balance of fluid movement. Fluids and electrolytes continually shift, primarily because of osmosis from a low- to a high-sodium concentration. Fluids between all of these compartments are under a continual dynamic equilibrium. The electrolyte composition of ICF and ECF are very different and play a key role in fluid balance. 3 The interstitial area is the space between cells where fluid is held in a gel-like form in a proteoglycan/collagen matrix. 3 Approximately three fourths of the ECF consists of ISF, with the remaining fourth being IVF. 3 ECF is composed of both interstitial fluid volume (ISF, ~15%), transcellular fluid (~1%), and intravascular fluid volume (IVF, ~5%). 1 Two-thirds (about 40%) of the total body water is stored in cells within the intercellular fluid (ICF), and one third of total body water is stored in the extracellular fluid (ECF). Total body water in a normal-weight dog is estimated to be 534 to 660 mL/kg.
2 Fatty tissue contains much less water than do muscle, organs, and soft tissue, so overweight animals tend to carry less water per pound proportionally to lean dogs. Very young dogs and cats have as much as 70% to 80% total body water, 2 while older pets may have as little as 50% to 55%. 1 The variation is often attributed to the patient’s age and nutritional status. In dogs and cats, body water averages 60% of their body weight. Having a fundamental understanding of the physiology of body fluids is key in treating patients and understanding fluid calculations.Īn understanding of total body water volumes aids in fluid therapy: for example, knowing that fluid loss from young puppies takes a much higher percentile of their body weight, making fluid replacement vital, and, conversely, understanding that fluid administration to an obese patient may need to be based on their lean or ideal body weight rather than their actual weight.
Body fluid compartments calculations how to#
We will explore the physiology of body fluids, how to assess a fluid imbalance, administering and monitoring fluid therapy, and various types of fluids. Inappropriate fluid therapy may result in overhydration or fluid overload, electrolyte deficiencies, acid/base imbalances, rapid fluid shifting, and potential complications of IV catheter use. Technicians need to understand these intricate processes in order to properly assess, administer, and monitor fluid therapy.
Fluid therapy can be used for a variety of reasons including: treating shock, blood loss, and dehydration preventing dehydration treating systemic disease providing supportive care during anesthesia and providing diuresis. A variety of diseases, conditions, and surgical interventions can disturb this balance. Fluid balance, electrolyte balance, and acid-base balance work together to maintain homeostasis within the body. Maintaining a proper fluid balance in the body is essential to life and the patient’s longevity. Usually, though, veterinarians do the calculating, don’t they? Is it important for veterinary technicians to cultivate these skills? A variety of veterinary calculators are now available to calculate fluid estimates for the patient, but knowledge of how to properly calculate fluids is vital for veterinary technicians to develop and maintain because it deepens the understanding of the patient’s condition. Finally, the regulation of sodium is discussed with examination of the mechanisms controlling natriuresis and the reciprocity with potassium balance.Fluid calculations are part of daily life in modern veterinary practice. The endogenous processes contributing to volume homeostasis are then deliberated including the detection of fluid imbalance through intracellular and extracellular systems as well as the hypothalamic and renal effector mechanisms. The way in which clinically administered fluids of varying compositions affect the fluid compartments is subsequently discussed. To illustrate daily fluid balance in a healthy individual, a typical intake and output over 24 hours is quantified before consideration of iatrogenic contributions to this equilibrium. The differences in ionic concentration between intracellular and extracellular fluid are quantified and the effects of greater relative protein concentration within cells are also considered.

Furthermore, the potential disadvantages to the approach are discussed. Here, the calculation of these volumes by measuring the dilution of markers able to permeate specific compartments is considered. The dynamic balance across these compartments is an essential component of normal physiology. The water contained in the body is divided amongst compartments of differing sizes and compositions.


 0 kommentar(er)
0 kommentar(er)
